- Published on
Sepsis biomarkers: A review.
- Authors
- Name
- Jake Konigsberg
- Role
- Founder
Pierrakos, C. & Vincent, J.L., (2010). Sepsis biomarkers: A review. Critical Care 14 https://doi.org/10.1186/cc8872
Summary:
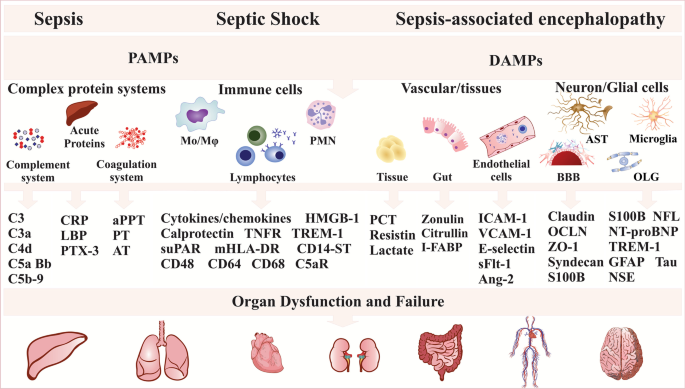
Sepsis is a leading cause of death in critically ill patients despite modern methods of treatment. Due to the complex and severe nature of the condition, early diagnosis and treatment are necessary to provide the best chance of survival; however, it is difficult to diagnose sepsis due to its various signs and symptoms. Therefore, identifying biomarkers that can be used to indicate the presence and severity of sepsis is necessary. Biomarkers can also help identify the root of septic conditions whether it be from bacterial, viral, or fungal infection. Biomarkers can also be used to assist in the treatment of sepsis by guiding antibiotic therapy and evaluating the response to therapy and recovery. However, without a current good biomarker for sepsis, it remains difficult to differentiate sepsis from other causes of systemic inflammatory response syndrome. Therefore, this paper focused on analyzing 3370 studies that assessed a biomarker in sepsis, specifically evaluating a total of 178 different biomarkers.
A favorable biomarker for the treatment of sepsis has sensitivity, alterations in levels indicative of the presence of sepsis, and specificity, providing information about the state and severity of the septic condition. While many biomarkers were analyzed for sepsis, none were both sensitive and specific. For example, PCT, acute phase proteins, have been extensively used yet lack both specificity and sensitivity. Cytokines, molecules involved in the inflammatory response which act upon immune cells, have also been considered as possible biomarkers, but while they have sensitivity, they lack specificity as their levels are rather erratic.
The diagnosis of sepsis and identification of a quality biomarker is difficult, and an ideal biomarker is still lacking. One suggestion has been combining several biomarkers, but further study is required.
Implications:
Future studies should focus on testing the combination of various biomarkers to craft a specific and sensitive model for the diagnosis and treatment of sepsis. The complex and diverse nature of sepsis makes it difficult to identify a single type of biomarker, but if and once one is identified, it will allow for the early identification and quick treatment of sepsis essential in preventing its progression and enhancing one’s odds of survival.