- Published on
Pathophysiology, clinical presentation, and treatment of psoriasis
- Authors
- Name
- Amanda Liswood
- Role
- Research Coordinator
Source:
Armstrong, A. W. (2020). Pathophysiology, clinical presentation, and treatment of psoriasis: A review. JAMA, 323(19), 1945-1960. DOI: 10.1001/jama.2020.4006
Summary:
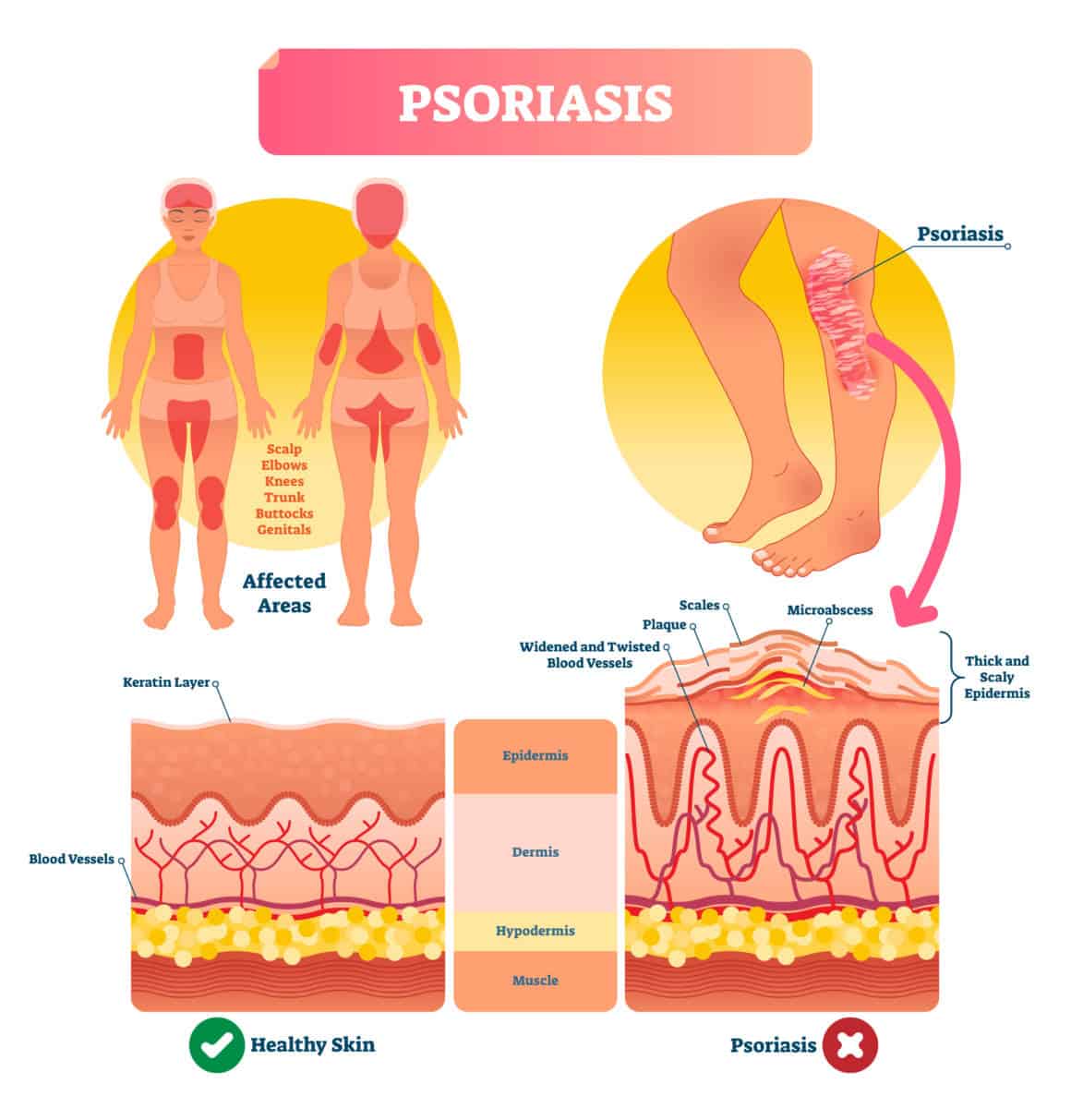
125 million people in the world suffer from the chronic skin disease called psoriasis. The central cause of psoriasis is thought to be the excessive activation of the adaptive immune system due to the unregulated release of pro-inflammatory cytokines (messengers) by immune cells. These molecules act by stimulating myeloid dendritic cells (cells responsible for activating an immune response by processing an antigen and then presenting it to immune cells), leading to the production and differentiation of T-cells (a cell type which plays a role in the adaptive immune response) resulting in an inflammatory cascade. This continuous chain of reactions ultimately causes immune cells to infiltrate the skin leading to itchy patches characteristic of psoriasis.
The risk factors for psoriasis are genetic, environmental, and behavioral. Genetics factors are the most prominent with psoriasis involving multiple genes which mutations can increase one’s risk of getting the disease. Environmental and behavioral factors are also at play such as skin trauma and smoking.
There are many different types of psoriasis. 80-90% of those with psoriasis have plaque psoriasis which is presented as scaly patches often found on the scalp, trunk, and extensor surfaces (ex: elbows and knees). Other less common psoriasis types include guttate psoriasis (2% of psoriasis patients), erythrodermic psoriasis (2-3% of psoriasis patients), and pustular psoriasis.
Guttate psoriasis– Many confetti-like, pink scaly patients
Erythrodermic psoriasis– Large-scale reddening, scales or exfoliation involving at >75% of the body
Pustular psoriasis– Sterile pustules and reddening
Over the past several years, there has been significant research in understanding psoriasis genetics, comorbidities (such as arthritis), and biologic treatments. The most common treatments for mild or localized psoriasis patients are topical agents, such as corticosteroids. These treatments involve reducing the quantity of cellular products produced from genes encoding pro-inflammatory messengers serving to reduce inflammation. When the psoriasis progresses to moderate or severe, which is defined as covering approximately 3-10% of the body surface area, biologics have become the most common form of treatments. Biologics are further discussed in our blog about psoriasis treatments and work by inhibiting the production of pro-inflammatory messengers.
Implications:
This literature review discusses the pathogenesis, clinical presentation, risk factors, comorbidities, and treatments associated with psoriasis. This paper serves as an informative overview of the disease, especially for a patient who was recently diagnosed with psoriasis. Unfortunately, psoriasis diminishes quality of life through its risks and symptoms, and thus novel treatments and possible cures are currently being researched.